October 29th is recognized as World Psoriasis Day, which has annually been dedicated to people suffering from psoriasis and psoriatic arthritis. Besides giving the psoriasis community a voice, this day is used to raise awareness, spread accurate information, and improve access to treatment for patients. This year, the International Federation of Psoriasis Association, or IFPA, is dedicated towards the message of “treating psoriasis seriously.”
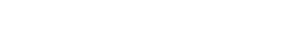
Psoriasis as such is a chronic inflammatory skin condition. Affecting around 2-4% of the population, it is most often characterized by thick scaling red plaques involving skin and nails. These plaques vary in size, morphology and distribution. These lesions usually cause patients to experience itching, stinging, and pain at different levels of severity.1,2 After learning about these symptoms, it is not difficult to understand why we need to take these conditions seriously.
One important issue that needs attention is the psychological effect that carrying the disease might have on patients. Psoriasis is a lifelong disease that has a low mortality and high morbidity. Because of this, other issues can arise such as psychosocial disabilities. This can significantly affect a patient’s quality of life.1,2 In fact, depression and suicidal ideation is prevalent among cosmetically disfiguring dermatological disorders. Additionally, when compared to other dermatology patients, patients with psoriasis and acne have been found to have the highest prevalence of suicidal ideation.3-5
…compared to other dermatology, patients with psoriasis and acne have been found to have the highest prevalence of suicidal ideation.
There are presently many treatment options available for psoriasis patients. The availability and usage of biologic treatments are increasing, but the main treatment of choice is topical therapies. Although there are a variety of options, dermatologists in key markets such as US, Japan, and the EU5 are highlighting that there needs to be an increase in lower-cost biologics for patients. They also suggest better reimbursement protocols in these same regions. 6-10
Taking these topics into consideration, we strongly encourage a continuous growth in psoriasis awareness and the other issues that the condition might cause patients, such as psychosocial disabilities. We also hope to see improved patient access to both appropriate and affordable treatment options.
References
1. Armstrong, A.W. et al. 2012. The association between psoriasis and obesity: a systematic review and metaanalysis of observational studies. Nutr Diabetes, Dec 3;2:e54. 2. Parisi, R. et al. 2013. Global Epidemiology of Psoriasis: A Systematic Review of Incidence and Prevalence. J Invest Dermatol, 133(2):377–385. 3. Gupta, M.A. and Gupta, M.K. 1998. Depression and suicidal ideation in dermatology patients with acne, alopecia areata, atopic dermatitis and psoriasis. Br J Dermatol, Nov;139(5):846-50. 4. Voorhees, A.V. and Fried, R. 2009. Depression and Quality of Life in Psoriasis. Postgraduate Medicine, 121:4, 154-161 5. Chimenti, S. et al. 2006. An Italian Study on Psoriasis and Depression. Clinical and Laboratory Investigations, 212:123-127. 6. Bhutani, T. et al. 2013. Access to health care in patients with psoriasis and psoriatic arthritis: Data from national psoriasis foundation survey panels. JAMA Dermatology, 149:717–21. 7. van Cranenburgh, O.D. et al. 2013 Psoriasis patient’s satisfaction with treatment: a webbased survey study. Br J Dermatol, 169(2):398–405. 8. Cheng, J. and Feldman, S.R. 2014. The cost of biologics for psoriasis is increasing. Drugs Context, Dec 17;3:212266. 9. Takeshita, J. et al. 2015. Psoriasis in the U.S. Medicare population: prevalence, treatment, and factors associated with biologic use. J Invest Dermatol, 135(12):2955–63. 10. Gottlieb, A.B. et al. 2016. Psoriasis trends and practice gaps. Dermatologic Clinics, 34(3), 235–42